Cervical Cancer
Cervical cancer is the leading cause of cancer death among women in 29 countries in sub-Saharan Africa.
Cervical cancer is preventable, owing to effective primary prevention via human papillomavirus (HPV) vaccination and secondary prevention via screening. However, it remains the fourth most common cancer and the third leading cause of cancer death in women worldwide, with 662,000 new cases and 350,000 deaths estimated in 2022. There is a 45-fold difference in cervical cancer incidence rates across countries (Figure 17.1) due to uneven progress made against the disease (Figure 17.2).
Cervical cancer incidence, age-standardized rate (world) per 100,000, in selected countries, 2022
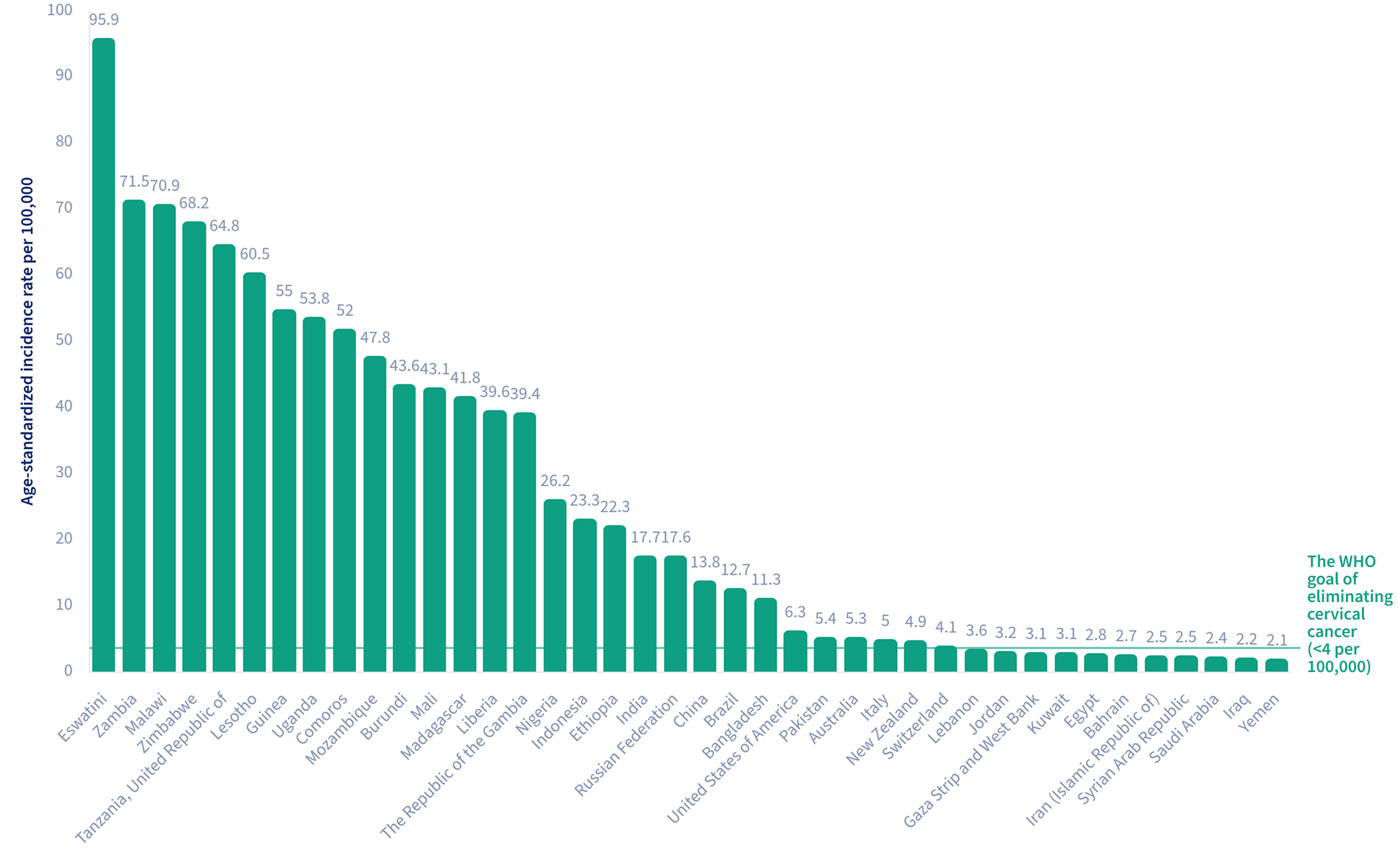
Uneven declines in cervical cancer incidence across countries highlight persistent global inequities in cancer prevention efforts.
Trends in cervical cancer incidence, age-standardized rate (world) per 100,000, 1960-2020
Efforts to reduce the cervical cancer burden are particularly critical in sub-Saharan Africa, where incidence rates are the highest in the world (Figure 17.1) and the disease remains the leading cause of cancer death in women in 29 countries (Map 17.1).
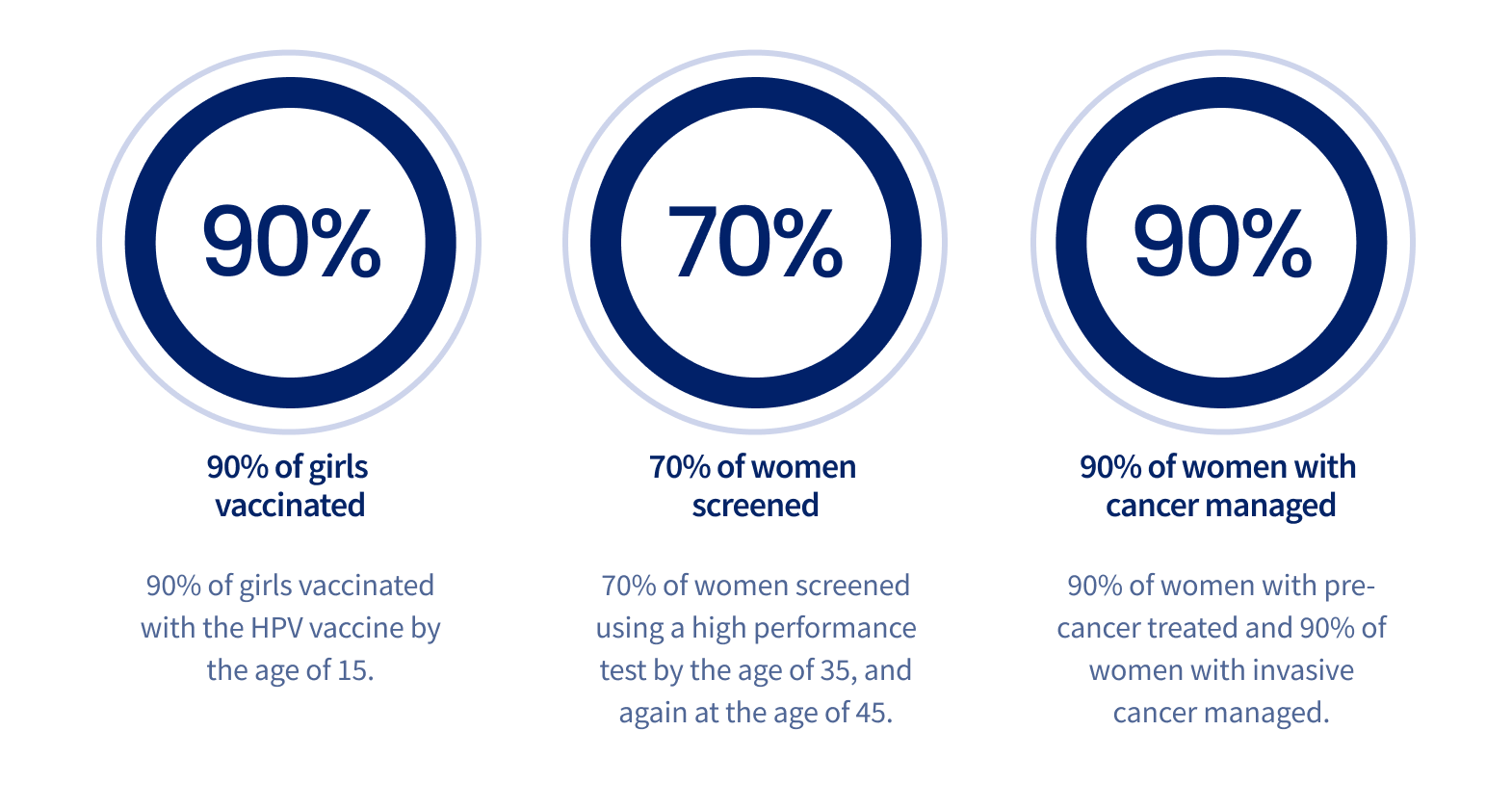
To achieve the goal of incidence rates of less than four per 100,000 women set by the World Health Organization (WHO) Cervical Cancer Elimination Initiative (CCEI), each country should meet the 90-70-90 targets aiming at 90% of age-eligible girls being HPV-vaccinated, 70% of age-eligible women having ≥1 lifetime cervical screening, and 90% of women with precancerous and cancerous cervical lesions being treated effectively, by the year 2030 (Figure 17.3).
The 2030 targets of the World Health Organization Cervical Cancer Elimination Initiative (CCEI)
Nevertheless, by 2019, nearly two decades after the HPV vaccines were recommended by the WHO, only 1% of girls in Northern Africa and Western Asia were vaccinated (first dose), compared with 86% in Australia and New Zealand (see Vaccination, Figure 35.2). In 2019, only one in three women aged 30-49 years had ever been screened for cervical cancer, and 63 of 202 countries did not have official screening recommendations as of 2021. In 2023, the high-performance HPV detection-based screening has been rolled out in only 19 countries, all of which are high-income countries (see Early Detection, Map 36.1).
“For the first time, the elimination of a cancer is within our reach.”
Single-dose HPV vaccination reduces cost and simplifies implementation of HPV vaccine programs, while HPV-based cervical screening, paired with self-collected cervical samples, improves risk-stratification and increases screening access in remote and underserved areas. As of April 2025, 68 countries recommend single-dose HPV vaccination. Cervical cancer is an extreme example of a global health disparity. Dramatic progress is needed. Targeted efforts to implement cervical cancer prevention measures are key to reducing disparities in cervical cancer incidence and mortality worldwide.