Ultraviolet Radiation
Up to 90% of melanomas are attributable to harmful sun exposure.
Ultraviolet radiation (UVR) is the principal cause of common skin cancers: keratinocyte cancers (basal cell and squamous cell carcinomas, referred to as non-melanoma skin cancer in the remaining chapters) and cutaneous melanomas. Each year, more than 332,000 new cases of melanoma occur globally, resulting in more than 59,000 deaths. It is estimated that 70-90% of cutaneous melanomas and virtually all keratinocyte cancers are attributable to UVR exposure.
“I will never choose between UV protection and beauty again.”
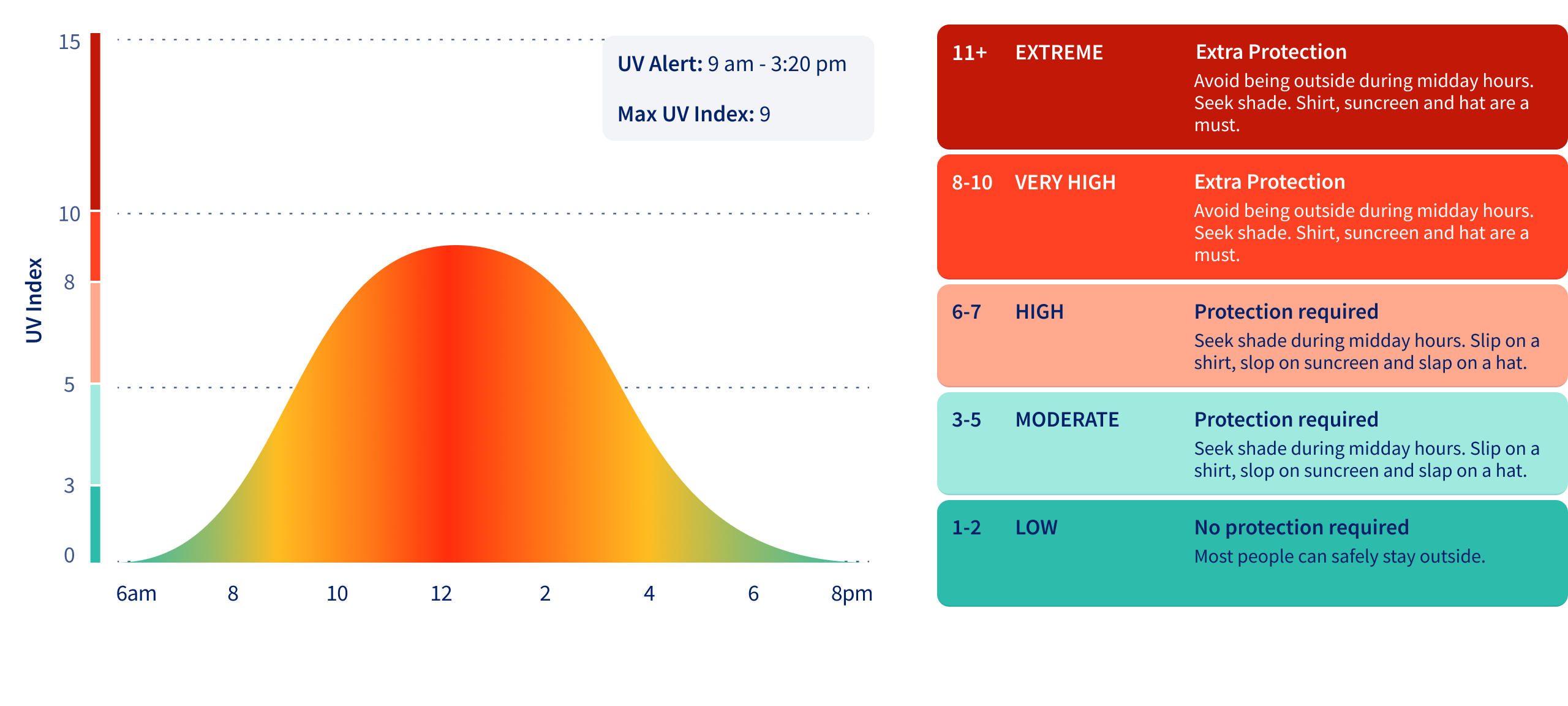
The UV Index describes the intensity of solar UVR. The UV Index varies according to the time of day (it is highest at noon), season of the year (highest in summer), and latitude (highest at the equator) (Figure 8.1). The highest UV Index readings are recorded in the tropics, particularly at high altitudes where the atmosphere is thin.
People who start indoor tanning before the age of 35 have a 60% higher risk of melanoma.
Ultraviolet (UV) index and sun protection recommendations
“If you could see radiation, you’d protect your skin more.”
Most people are exposed to UVR from the sun, although some people receive high doses from artificial sources including solaria (tanning beds) and welding equipment. The high-energy photons of UVR penetrate the skin’s outermost layers and cause genetic mutations in the deeper cells that serve to replenish the skin. This damage can ultimately progress to cancer. Melanin pigments in the skin provide some natural protection to skin cells from the harmful effects of UVR.
The highest incidence of skin cancer is observed among light skinned populations residing in regions that experience high UV Index throughout the year (Map 8.1). Patterns of melanoma incidence appear to be changing in some regions as a consequence of migration and population admixture.
Primary prevention of skin cancer aims to reduce population exposure to all sources of UVR. Long-running campaigns in Australia (which has the world’s highest rates of skin cancer) recommend the public to protect themselves from sun exposure when the UV Index is forecast to be 3 or more by wearing protective clothing, sunglasses and hats, seeking shade, and applying sunscreen to all exposed skin (Figure 8.2). In addition, many jurisdictions have banned solaria (at least for young people), and sun-safe policies are being promoted in schools, workplaces, and recreational settings.