Building Synergies
Cancer research anywhere should benefit cancer patients everywhere.
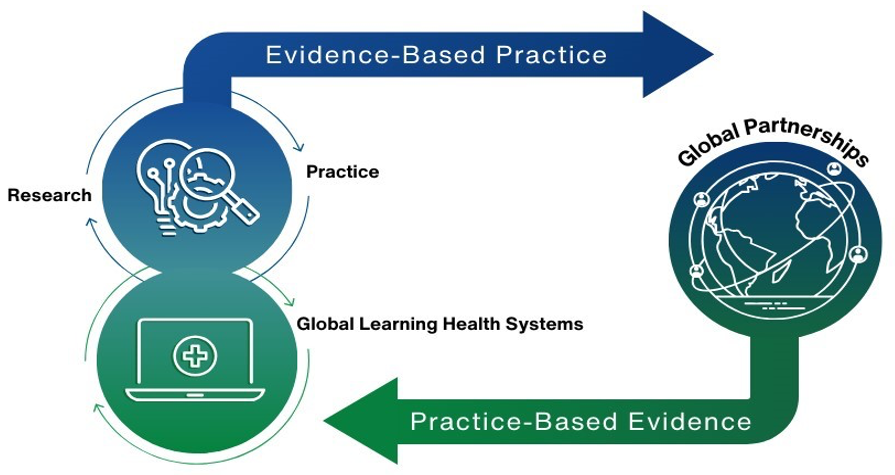
Global cancer control requires a coordinated response from national governments, researchers, funders, practitioners, advocates, patients, and international organizations. Multiple high-level resolutions have called for reduced cancer mortality, but work remains to meet targets and understand what approaches work best, especially in low- and middle-income countries (LMICs), where burden is increasing. Synergies created through equitable partnerships and networks are critical, coupled with strong research investment and implementation of emerging evidence. Connecting researchers with policymakers, practitioners, civil society, and people with lived experience ensures that policies and practices are evidence-based and that cancer research addresses real-world needs and experiences. This feedback loop allows all voices to be heard and cancer discoveries to reach populations who have been historically excluded (Figure 42.1).
Research to practice & policy feedback loop
Synergies across researchers and implementers are exemplified by the creation of integrated person-centered services to address non-communicable diseases in LMICs. In Zambia, human papillomavirus vaccination has been integrated in human immunodeficiency virus (HIV) clinics to reach national targets. Rwanda, for example, has integrated non-communicable diseases services in rural HIV clinics.
Additionally, a well-trained cancer workforce is essential. The US National Cancer Institute (NCI) and many other organizations, such as the African Organization for Research and Training in Cancer (AORTIC), Latin American and Caribbean Society of Medical Oncology (SLACOM), American Society of Clinical Oncology (ASCO), and others, support training and career development (Map 42.1). These programs, led by individuals or organizations around the world, leverage existing research collaborations and infrastructure, including those established for HIV, to build a rich global cancer workforce and ecosystem globally.
The International Cancer Control Partnership (ICCP), a group of more than 20 partner organizations and UN agency partners, convened by the US NCI and the Union for International Cancer Control, has focused on supporting and learning from countries as they navigate the process of national cancer-control plans implementation (Map 42.2).
“We know that without continuous reflection, stakeholder engagement and recalibration, we cannot hope to be successful in meeting our shared goals and closing the [cancer] care gap around the world.”
Cancer planners in countries build synergies across diverse partners and disciplines including academic, clinical, advocacy, and policy to achieve national objectives (Figure 42.2). ICCP works to expand analogous collaborations globally to enable cancer control at local, national, regional, and international levels.