Cancer Survival
Access to effective early detection and cancer treatment can substantially improve survival for cancer patients and reduce the survival gap worldwide.
Overall improvements in early detection and treatment have greatly improved average survival of cancer patients worldwide over the past several decades, yet prognosis still varies markedly depending on where a patient lives. (Figure 1) Survival differences are also marked within regions. Within sub-Saharan Africa for example, overall (observed) survival of women diagnosed with breast cancer is about 50% higher in patients residing in high Human Development Index (HDI) countries than in those residing in low-HDI countries. (Figure 2) This is in part because breast cancer patients in the low-HDI countries are more likely to be diagnosed at a later stage and less likely to receive the appropriate treatment. In addition to variation between countries, within-country differences have also been reported. For example, in the United States, black cancer patients have lower survival than non-Hispanic white patients. (Figure 3)
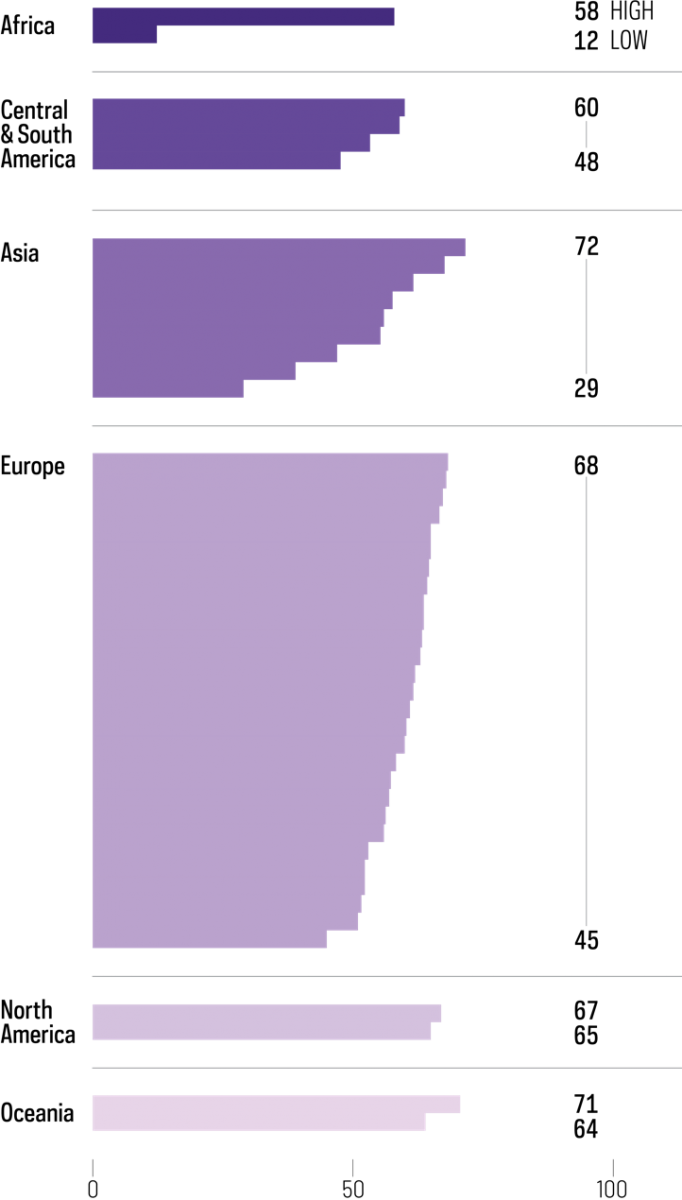
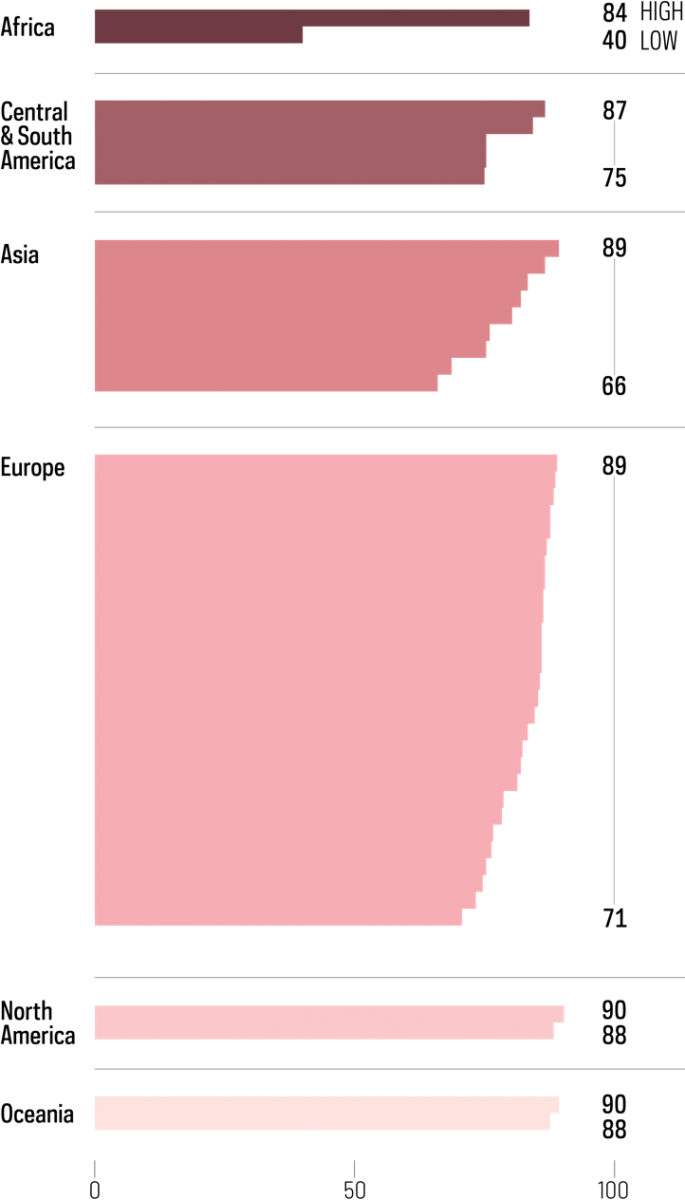
Figure 1. Five-year net survival (%) in patients diagnosed with colon cancer, female breast cancer, and acute lymphoblastic leukemia (children) in 2010–2014 CONCORD-3 study worldwide. Colon cancer five-year survival: In Africa, ranges from 12 to 58%. In Central and South America, ranges from 48 to 60%. In Asia, ranges from 29 to 72%. In Europe, ranges from 45 to 68%. In Northern America, ranges from 65 to 67%. In Oceania, ranges from 64 to 71%. Female breast cancer five-year survival: In Africa, ranges from 40 to 84%. In Central and South America, ranges from 75 to 87%. In Asia, ranges from 66 to 89%. In Europe, ranges from 71 to 89%. In Northern America, ranges from 88 to 90%. In Oceania, ranges from 88 to 90%. Childhood acute lymphoblastic leukemia five-year survival: In Central and South America, ranges from 50 to 69%. In Asia, ranges from 58 to 89%. In Europe, ranges from 54 to 95%. In Northern America, ranges from 90 to 93%. In Oceania, ranges from 91 to 91%.
Figure 2. Observed survival (%) in patients with breast cancer since time of diagnosis in countries with high, medium and low human development index in sub-Saharan Africa in 2009–2014. High HDI includes Seychelles, Mauritius. Medium HDI includes Kenya, Namibia and South Africa. Low HDI includes Benin, Côte d’Ivoire, Ethiopia, Mali, Mozambique, Uganda and Zimbabwe. In high-HDI sub-Saharan African countries, breast cancer survival declines to 71% at five years after diagnosis. In medium-HDI sub-Saharan African countries, breast cancer survival declines to 46% at five years after diagnosis. In low-HDI sub-Saharan African countries, breast cancer survival declines to 42% at five years after diagnosis.
Figure 3. Five-year net survival (%) for women diagnosed with advanced breast cancer in the USA in 2009–2015 by race/ethnicity. Five-year net survival is 31.2% for Hispanics (of any race); 31.2% for Asians and Pacific Islanders (includes Hispanic); 28.2% for non-Hispanic whites; and 19.7% for blacks (includes Hispanic).
In order to close this survival gap, improved population awareness about cancer symptoms, better access to diagnostic services, and adequate care are key. Universal Health Coverage is one strategy to achieving this. (see Universal Health Coverage) The implementation of universal health coverage in Thailand in 2002 may at least partly account for the increase in the 5-year breast cancer survival proportion, from 44% for patients diagnosed from 1995 to 1999 to 62% for those diagnosed from 2010 to 2014. (Figure 4)
Figure 4. Trends in five-year net survival (%) from breast cancer in Asia. In Singapore, five-year breast cancer survival increased from 76% in 2000-2004 to 80% in 2010-2014. In Penang, Malaysia, five-year breast cancer survival increased from 65% in 1995-1999 to 74% in 2005-2009 before declining to 65% in 2010-2014. In Thailand (6 registries), five-year breast cancer survival declined from 66% in 1995-1999 to 57% in 2000-2004 before increasing to 69% in 2010-2014. In India (two registries), five-year breast cancer survival increased from 48% in 1995-1999 to 66% in 2010-2014
Cancer patient survival benchmarking is an important tool for advocacy to ensure equitable cancer care. Global initiatives assessing international cancer survival include EUROCARE, a cross European project since 1989; the International Cancer Benchmarking Partnership, involving high-income countries with similar health systems; CONCORD, which collects and reports data from all countries worldwide; and SURVCAN, which aims to improve data and capacity for survival estimation in Africa, Asia, and South America, including an initiative with the African Cancer Registry Network to expand population-based survival estimates in sub-Saharan Africa. Unfortunately, high-quality data remains scarce. (Map 1) Improving the quality and availability of population-based survival data is essential to ensuring effective monitoring of progress in cancer control.
ACCESS CREATES PROGRESS
The number of population-based cancer registries that are able to provide high-quality survival statistics is lacking but has grown over the last decades, providing national and global evidence to improve effectiveness of health care systems.
Net survival is a measure of the probability of surviving the cancer diagnosed that is comparable between countries, as it corrects for differences between countries in death from other diseases (non-cancer mortality). Net survival is often age-standardized for comparability between countries with different age distributions.
Observed survival is a measure of the probability of a person with cancer surviving from all causes of death (cancer and other causes).
Survival from childhood acute lymphoblastic leukemia:
Allemani C, Matsuda T, Di Carlo V, et al., for the CONCORD Working Group. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018 Mar 17;391(10125):1023–1075.
Access creates progress:
ibid.
Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385: 977–1010.
Text:
Allemani C, Matsuda T, Di Carlo V, et al., for the CONCORD Working Group. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018 Mar 17;391(10125):1023–1075.
SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute. Available from https://seer.cancer.gov/explorer/.
Joko-Fru WY, Miranda-Filho A, Soerjomataram I, et al. Breast cancer survival in sub-Saharan Africa by age, stage at diagnosis and Human Development Index (HDI): A population-based registry study. Int J Cancer. 2019. doi: 10.1002/ijc.32406 CC license BY-NC 4.0
Map:
Data quality varies according to cancer site and is typically better for more common cancer sites. Data quality determination in the map is based on breast cancer data.
Allemani C, Matsuda T, Di Carlo V, et al., for the CONCORD Working Group. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018 Mar 17;391(10125):1023–1075. Licence CC BY 4.0
Additional data provided by the SURVCAN project: http://survival.iarc.fr/Survcan/en/
Figure 1 and 4:
Adapted from Allemani C, Matsuda T, Di Carlo V, et al., for the CONCORD Working Group. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018 Mar 17;391(10125):1023–1075. Licence CC BY 4.0
Figure 2:
Joko-Fru WY, Miranda-Filho A, Soerjomataram I, et al. Breast cancer survival in sub-Saharan Africa by age, stage at diagnosis and Human Development Index (HDI): A population-based registry study. Int J Cancer. 2019. doi: 10.1002/ijc.32406 CC license BY-NC 4.0
Figure 3:
SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute. Available from https://seer.cancer.gov/explorer/.